
A question I have commonly received is, which is worse, high blood sugar or low blood sugar? The short answer to that is low blood sugar is worse in the short term and high blood sugar is worse in the long term.
And for the long answer…this is part two dedicated to explaining high blood sugar or hyperglycemia.
If you haven’t read part one yet about low blood sugar, check that out here!
To start out with, let’s review overall blood sugar regulation.
The pancreas is continually monitoring the concentration of glucose in the blood. When it senses that it’s too high, it secretes insulin so that the glucose can exit the blood stream and enter into the cells to be used for energy. When it senses it’s too low, it secretes another hormone called glucagon which signals the liver to release stored glucose into the blood. This entire process is a continuous cycle to maintain blood glucose levels in a normal range.
High blood sugar or hyperglycemia is a failure point in the blood glucose regulation process brought on by managing and having diabetes just as low blood sugar or hypoglycemia is.
High Blood Sugar (Hyperglycemia)
A number of things can cause hyperglycemia. For those with type 1 diabetes, the most common cause is not having administered enough insulin leaving excess glucose in the blood stream and unable to enter the cells. For those with type 2 diabetes, there may be enough insulin, but it is not as effective as it should be. Other reasons contributing to high blood sugar are eating more than planned, exercising less than planned, stress from illness, stress from work, school, relationships, or dawn phenomenon (a surge of hormones produced in the body occurring daily around 4 or 5am) [1].
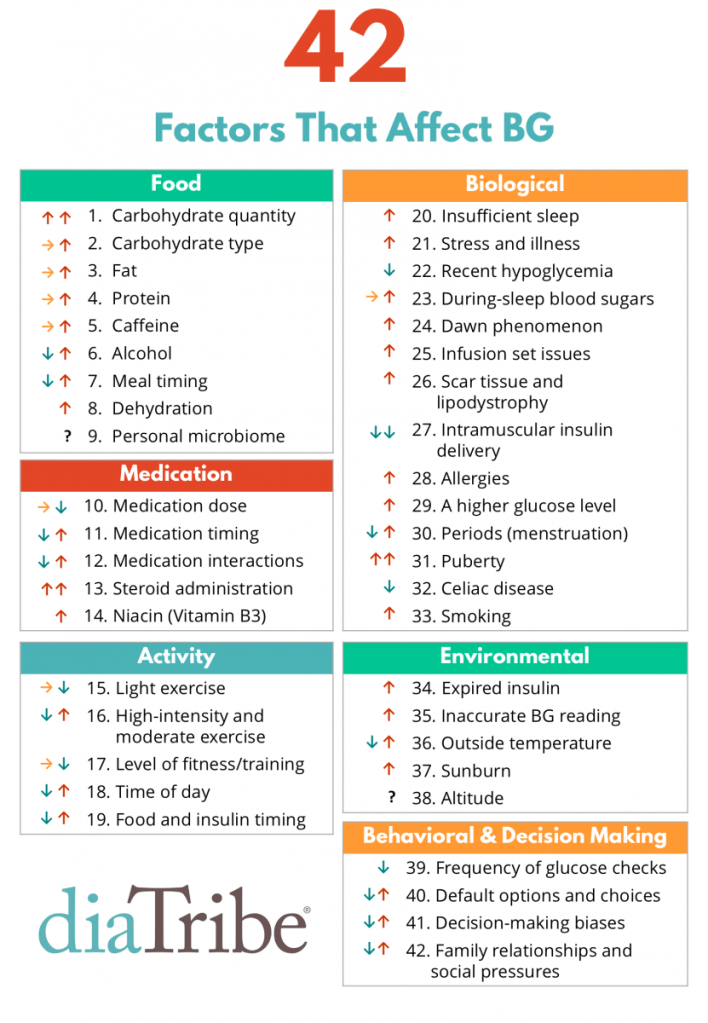
Check out the image below for a list variables that can affect blood sugar. There are a lot! This extensive list of variables is what makes managing diabetes challenging in figuring out how you specifically react to these factors. For me personally, I’ve noticed that dehydration, stress, and insufficient sleep greatly contribute to higher blood sugars.
The most common symptoms of high blood sugar include increased thirst and frequent urination (remember, the body is attempting to eliminate the excess glucose), but other symptoms include dry mouth, fruity smelling breath, headache, fatigue, and the feeling of a “mental fog.” For me personally, I first notice dry mouth and increased thirst when my blood sugar goes high with the onset of a headache and the mental fog if it is a prolonged high. There also exists what is known as the “diabetes hangover” where a severe high (or low as well) can trigger headache, fatigue, nausea, and other symptoms similar to an alcohol hangover. If I have a severe low or high throughout the night, I usually wake up not feeling good and it may last the entire day. These types of symptoms are what motivates me (and I hope others as well!) to try my best at maintaining consistent blood sugar levels as all the “ups and down” can leave you feeling like crap to say the least.
The American Diabetes Association generally recommends the target blood sugar levels of:
- Between 80 and 130 mg/dL (4.4 and 7.2 mmol/L) before meals [6]*
- Less than 180 mg/dL (10 mmol/L) two hours after meals [6]*
Target blood sugar ranges can vary by person meaning what is considered “high” will vary by person as well. In contrast to low blood sugar which has a relatively small range (i.e. roughly 50-70 mg/dL), high blood sugar has a large range starting from around 180-200 mg/dL* and up. The highest I have ever been that I can recall was in the 500s mg/dL. Onset of high symptoms begin around the 180-200 mg/dL* with usually the feeling of increased thirst. As blood sugar continues to rise, symptoms will become more severe and can ultimately result in DKA.
*Target ranges and what is considered a high blood sugar for when intervention should occur can vary by person and should be discussed with your medical team. For example, a pregnant woman with type 1 diabetes who needs to have very tight control may consider a blood sugar over 140 mg/dL as high but for a young child who can drop quickly and has high insulin sensitivity, blood sugar may not be considered high until over 200 mg/dL.
Diabetic Ketoacidosis (DKA)
Diabetic Ketoacidosis, or DKA for short, starts to become a concern usually when blood sugar levels pass the 250 mg/dL mark and is signaled by the onset of nausea and vomiting in addition to the other symptoms mentioned previously.
Keep it Simple for Me! Explanation: Without insulin, the body cannot use glucose for fuel so it moves to accessing it’s secondary energy source of breaking down fat for fuel. A byproduct of breaking down fat is the creation of a ketone. A ketone is an acidic molecule and the body cannot tolerate large amounts of ketones. If ketones are not eliminated quick enough through the urine, they build up in the blood and decrease the body’s pH level creating a toxic state for the body known as ketoacidosis. This is a life-threatening situation that needs immediate medical attention [1].
Nerd Alert! Explanation: A lack of insulin shifts the body into thinking it is in a period of starvation because glucose is not able to move into the cell for energy production. The body begins to break down fat into it’s base component of amino acids which can then be used to synthesize glucose (gluconeogenesis) or ketones (ketogenesis). Ketones are produced in the liver and can be used as a direct source of energy by the muscles, brain, and kidneys as they have the enzymes needed to metabolize ketones for energy. While ketone production and use is a key survival mechanism of the body, ketone production can exceed ketone use. If excess ketones are not eliminated quickly enough through the urine, they begin to build up in the blood which is called ketosis. An indicator of ketosis is a fruity breath odor. Severe ketosis occurs when the level of ketones in the blood rises to the point of decreasing the pH level of the blood resulting in ketoacidosis. This is a toxic state for the body that can cause nausea and vomiting, coma, and in extreme circumstances, death [4]. Ketoacidosis is a life-threatening situation that needs immediate medical attention [1].
Hemoglobin A1c (HbA1c) and Long Term Complications
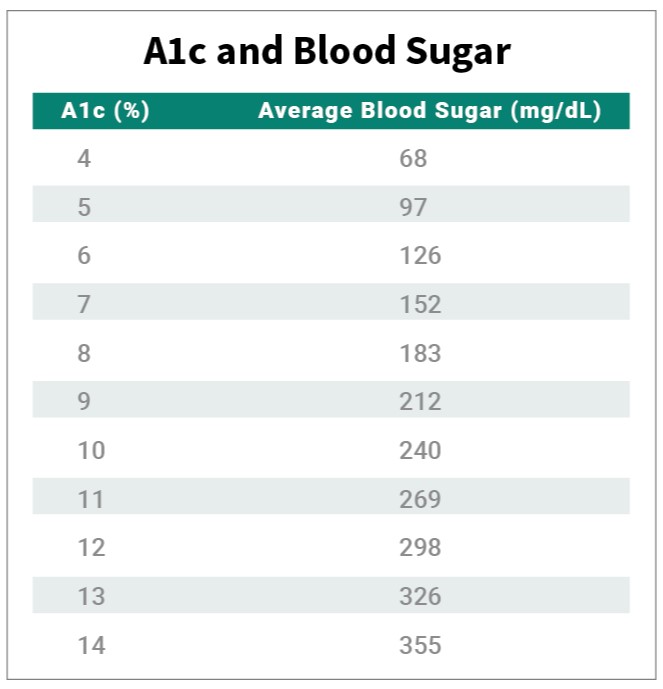
Another piece in addition to the amount of sugar in the blood is the amount of time the sugar in the blood stays at an elevated level. Hemoglobin is a protein found in red blood cells and is responsible for carrying oxygen throughout the body. When there is excess glucose in the blood, that glucose enters the red blood cell and binds to the receptors that are meant to carry oxygen resulting in the hemoglobin becoming glycated. The more excess glucose in the blood, the more glycated the hemoglobin becomes. The A1c test measures how much glucose is bound to the hemoglobin and provides an average blood glucose level over the past 3 months (red blood cells live for roughly 3 months) [2]. The American Diabetes Association suggests that an adult person with diabetes should target a HbA1c of below 7 to be considered well controlled, but A1c targets can change over time due to the person and their circumstances [3]. Your target A1c goal should be discussed with your diabetes care team.
In addition to A1c, time in range (TIR) is another key indicator to blood sugar management. To learn more about time in range check out this blog post. Here is a quick reference on A1c percentages correlated to an average blood sugar.
Sugar or glucose in excess can block blood vessels, weaken blood vessel walls, interfere with nerve signal transmission, damage nerves, and provide a breeding ground for bacteria. This is why those with diabetes are at increased risk for infections, skin complications, cardiovascular disease, high blood pressure, strokes, neuropathy (nerve damage), nephropathy (kidney disease), and eye complications such as glaucoma, cataracts, and retinopathy [5]. Most simply put, excess sugar in the body causes stress to the body structures and that compounds over time resulting in complications. This is why high blood sugar is worse in the long term (to answer the initial question that started this).
Treating High Blood Sugar (Hyperglycemia)
*Disclaimer: Management of high blood sugar should be discussed with your doctor and diabetes care team. The below information is my own personal experience or from a source where noted.
Singular High Episode:
- Drink lots of water! This will help to flush excess glucose out through the urine and address if dehydration may be contributing to the high blood sugar.
- Exercise! If your blood sugar is above 240 mg/dL, check for ketones before exercising as exercising with ketones can worsen the situation [1]. Exercise allows the muscle cells to directly uptake glucose from the blood stream without insulin (pretty cool right?!). On a side note, this is how exercise increases insulin sensitivity and a future blog post will be dedicated to this topic.
- Administer a correction dose of insulin! If it has been more than 2 hours since you last ate and no bolus insulin is onboard, administer a correction dose. Now, the hardest part here is having the patience to wait and not rage bolus. Yes, I said rage bolus. Fast-acting insulin peaks at about 1 hour with peak effectiveness at 2 hours. This means that if blood sugar is still high at 1 hour post correction dose, do not administer more as that initial dose has still not reached peak effectiveness. If do administer more insulin, that is then stacking on top of the initial correction dose and could then result in a low from having too much insulin. The “watch and wait” of managing a high blood sugar can be very frustrating. Again, addressing high blood sugar and correction insulin doses should be discussed with your diabetes care team to determine what is most appropriate for your diabetes management.
- If the above options are not working or the high blood sugar is persistent, then may need to change your pump site as the cannula may have gotten bent or perhaps the insulin went bad or maybe the pump site is in a spot with a lot of scar tissue so not getting good insulin absorption.
- Try to figure out the root cause of the high (easier said than done, right?). Identifying causes and patterns of highs can help prevent it from happening in the future or identify a need for a change in management strategies.
Long Term Highs or Patterns of Highs:
Long term highs or patterns of high blood sugar should be discussed with your diabetes care team as there are most likely more things at play rather than a singular event contributing to high blood sugar like not bolusing enough for something you ate, but here are a few suggestion on what those things might be:
- Basal Rate – If see that blood sugars steadily rise after not having eaten for a few hours, this may indicate that basal rates need to be modified or increased.
- Accuracy in Carbohydrate Counting – If see blood sugars spike after a meal and then stay steady without coming down, may need to analyze if appropriately counting the carbohydrates you are dosing for and/or taking into account fat and protein in the meal.
- Insulin to Carb (I/C) ratio – If carbohydrate counting is accurate and still see blood sugars spike after a meal and then stay steady without coming down, this may indicate a need to alter your insulin to carb ratio as may need more insulin per grams of carbohydrates.
- Timing of Bolus – If see blood sugars spike fairly drastically after eating but they do eventually return to normal range, you may need to examine the timing of your bolus to be earlier. Insulin has an onset time of about 15-20 minutes so pre-bolusing that amount of time in advance of eating can help prevent such a drastic spike in post meal blood sugars as your insulin has time to kick in before your food does. This is something I personally struggle with doing as I’m usually bolusing as I’m sitting down to eat, but we all have habits that are hard to break!
For those of you with diabetes reading this, I hope you have learned more about what contributes to high blood sugars and can also relate to similar experiences. I also hope you have learned more about ketones and ketoacidosis as this was a topic that I did not really understand for a long time.
For those of you without diabetes reading this, I hope you have learned more about another aspect of diabetes management that may help you support your loved ones living with diabetes and feel informed to know a person with diabetes is not doing drugs if they say they are high!
Thanks for reading and look forward to your questions and comments!
References (click the hyperlinks below to learn more about topics discussed throughout this post):
- American Diabetes Association (n.d.). Hyperglycemia (high blood sugar). American Diabetes Association. https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hyperglycemia
- WebMD (2020 November 6). Hemoglobin A1c (HbA1c) test for diabetes. WebMD. https://www.webmd.com/diabetes/guide/glycated-hemoglobin-test-hba1c
- American Diabetes Association (n.d.). A1C and eAG. American Diabetes Association. https://www.diabetes.org/diabetes/a1c-test-meaning/a1c-and-eag
- McGuire, M., Beerman, K.A., (2018). Nutritional sciences: from fundamentals to food (3rd ed.). Cengage Learning
- American Diabetes Association (n.d.). Complications. American Diabetes Association. https://www.diabetes.org/diabetes/complications
- Mayo Clinic Staff (2020 June 27). Hyperglycemia in diabetes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hyperglycemia/diagnosis-treatment/drc-20373635

Leave a comment